The Library of Terms
Easily transmitted through direct contact or the air; vaccination is recommended for all dogs that interact with other dogs in their neighborhood, boarding and daycare facilities, dog parks, and groomers.
Unvaccinated puppies or young dogs, and dogs that have a compromised immune system may experience severe symptoms.
Symptoms
- a dry, hacking cough
- “honking” cough
- nasal discharge
- decrease in appetite
- lethargy
- fever
A vaccine was developed to help protect dogs and is available if needed. It was found to not be contagious to humans.
Symptoms
The Influenza vaccine is given as a series of two, and then annually to adult and senior dogs.
The disease is spread through both direct and indirect contact.
Symptoms
For dogs, the vaccine offers protection from intestinal viruses including Distemper, Hepatitis, Parainfluenza, and Parvovirus.
For cats, the vaccine offers protection from upper respiratory viruses including Rhinotrachitis, Calicivirus, and Panleukopenia.
These vaccines are often abbreviated to DHPP and FVRCP.
Distemper vaccines are given as a series to puppies and kittens, annually to young adult pets, and every 3 years in older adults and seniors.
Nursing kittens, feral or outdoor cats, and cats living in multi-cat households are at risk of infection. There is currently no known cure for Feline Leukemia.
A blood work screen can be completed in hospital to determine if a patient is infected with Feline Leukemia.
Symptoms
There are many different types of flea and/or tick preventatives on the market today. We understand that it can be difficult to keep up with all of the brands, application methods, and pros/cons of them all. Here is a guide on the different types of preventives available with information about how they are applied, pros and cons for each one, and some things to think about when deciding if it is the right option for you and your pet.
When choosing a flea/tick preventative it is important to consider you and your pet’s lifestyle. There are many factors that could contribute to the decision of which option is best for you. Age, species, breed, health status, and any current medications should all be considered. All of the flea/tick preventatives are medications and any new products should not be started without first talking with your veterinarian.
The most popular form of flea/tick preventative is a topical medication, often referred to as “spot on” products. These are usually applied at the base of the neck or between the shoulder blades. They contain ingredients that kill fleas and ticks. Some products also contain a repellant quality that adds an additional layer of protection of keeping the pests off your pet in the first place. Topical preventatives spread over the pet’s body either through sweat glands or using a bioadhesive. It is generally convenient to use, and once dried, the pet is able to go swimming or be bathed. It is important to note that the product should be allowed to dry, and that it is important to keep kids and other pets away until fully dried. Also, be sure to bathe your pet with gentle shampoos that do not strip the skin. This could cause the medication to be removed as well. Possible side effects include itching/scratching, redness or swelling of the skin, or hair loss.
Oral medications are becoming more popular, as it takes away the worry of getting the topical medication on and letting it dry. None of the oral medications available have the ability to repel fleas or ticks, requiring the parasites to bite/attach before they will be killed. As with any oral medication, there is a risk of upsetting the stomach or the pet not taking the medication (either refuses to eat it outright or takes it and spits it out later… behind a couch). Possible side effects include vomiting and diarrhea, as well as some skin reactions like redness, itching, and/or hives. Depression and a decreased appetite have also been reported.
In addition to everything listed above, some topical and oral products can also prevent heartworm disease in dogs and cats. It is important to evaluate what each product covers to determine if you are getting the appropriate protection for your pet and their lifestyle
Collars are also popular since they can just be put on the pet and the owner doesn’t have to worry about a liquid product drying or giving the pet an oral medication. Collars contain a concentrated chemical that can kill and repel fleas and ticks. These are relatively inexpensive, but some of them can smell quite strong and can be irritating to the pet. There is also risk in humans touching the collars, especially children.
Sprays are also available, but can be difficult to apply for complete coverage. The pet has to stay dry for these to work also, which makes it difficult for baths, swimming, or even walking in the rain. It is important to remember when applying these to avoid the pet’s eyes and mouth.
Powders are dusted over the body and rubbed into the fur. Again, it can be difficult to get complete coverage and it is important to avoid the pet’s eyes and mouth. Side effects can include vomiting, diarrhea, drooling, depression, and decreased appetite.
Shampoos are available to help wash away adult fleas and their eggs. This is a very short-term solution and will not be a preventative measure. The pet can still get fleas later on. When using, you should allow it to sit on the skin and coat for at least 15 minutes before rinsing well. Be sure to avoid getting the shampoo in the pet’s eyes and mouth.
Dips are similar to shampoos, whereas they are not a preventative, but a short term solution. They are usually a very concentrated liquid that is diluted with water and applied to the pet. They do not get rinsed and need to be air dried. Dips cannot be used on very young pets or on pets if they are nursing or pregnant. It is usually advised to have a dip done by a professional, as they are very concentrated and should be used with extreme caution. If you are administering a dip, it is important to protect your skin and eyes while applying to the pet. You should also avoid the pet’s eyes and mouth.
Some important questions for you, as the pet owner to consider:
Tips for using a flea/tick preventative:
Heartworms are carried by several species of mosquitos and are transmitted when the mosquito feeds. When a bite occurs, the larval heartworms migrate through the soft tissue to the blood vessels and then they travel to the heart and lungs. Once there, they mature into adult worms, sometimes reaching several inches in length. The adult worms then reproduce, sending offspring into the bloodstream. The next mosquito that bites ingests the larva, becoming infected and carrying the parasite to its next host.
The classic form of heartworm disease occurs in dogs and is easily diagnosed with a blood test. Dogs with the disease often have large numbers of adult worms living in the blood vessels of the lungs and in the heart. These worms partially block the flow of blood, acting like a dam in the vessels. When the dog is active, it may have trouble moving enough blood to bring oxygen to the tissues. The heart must work much harder than normal to move the same amount of blood, and over time this leads to heart disease. Additionally, when adult heartworms are a few years old, they die of old age. Dead worms cause significant inflammation in the surrounding lung tissue, leading to coughing and shortness of breath. As the disease progresses, poor oxygenation and advancing heart failure can lead to the death of the dog.
Cats are not the normal host for heartworms, but recent studies show that they are infected at nearly the same rate as dogs. Cats also contract the disease through the bite of an infected mosquito. The heartworms start their migration through the tissue and blood vessels to the lungs, but often die in the lungs before reaching full maturity. If adult heartworms develop in a cat, it is usually in low numbers. Despite this fact, the migration of larval worms through the lungs can cause severe and permanent damage. Studies have shown that infected cats, even those in which the worms die before reaching maturity, develop long-term inflammation and narrowing of the airways. These cats may cough, show shortness of breath, or die suddenly due to their disease. Feline heartworm disease mimics, and is often misdiagnosed, as asthma. This is because the clinical signs and radiographic findings are identical, and heartworm tests do not consistently identify infected cats.
Dogs who contract heartworm disease can be treated with injectable medications. The treatment is expensive and painful, and even when the worms are gone, the lungs may be permanently scarred. To date, a safe treatment has not been developed for cats. The best “treatment” for both dogs and cats is to prevent the disease all together. Monthly heartworm prevention medications are available for both dogs and cats through your veterinarian. These preventatives are inexpensive, effective, and safe. All dogs and cats should receive monthly preventatives, even those who never go outside. This is because mosquitos commonly invade houses. Studies have shown that all indoor cats are at nearly equal risk for heartworm infection as cats that spend time outdoors. Additionally, monthly preventatives should be continued year-round because some species of mosquitos that transmit heartworm disease are hardy even in the middle of winter when there are sub-freezing temperatures.
In the Northern Virginia area, heartworm infection rates (as measured in dogs, where the test can accurately detect infection) are higher than they have been in the last 10 years. Your pet doesn’t have to be one of those infected. Protect your pet year-round with a heartworm preventative every 30 days. For more information on heartworm disease, visit The American Heartworm Society.
In dogs, heartworm tests work by detecting antigens of the heartworm in the dog’s blood. A few drops of blood are mixed with the test solution, and then poured into the tester. The tester contains antibodies that bind to heartworm antigens (a protein produced in the female worm’s uterus). When this binding occurs, a colored dot develops indicating the animal is infected with heartworms. Because infected dogs have a large number of heartworms in their system, these tests are very accurate. However, in order for a dog to test positive on the test, it must have mature female worms in its system. Heartworms take heartworm-interpreting-results courtesy of Idexxapproximately 6 months to reach maturity after infection, so dogs with very early infections may still test negative on the test.
There are two types of tests available for cats. One is an antigen test similar to the one used in dogs. This test will turn positive if it detects antibodies of three or more adult female worms. However, most infected cats only have a few adult worms in their system (1-7 worms), and chances are high that all or most may be male. If this is the case, the test will be negative. Thus, a positive antigen test in a cat indicates it is truly infected with heartworms, but a negative test does not rule out the possibility of infection.
The second type of test available for cats is an antibody test. This test detects heartworm-specific antibodies circulating in the cat’s blood stream. Antibodies are produced by the cat’s body when heartworm larvae reach the L4 stage. However, these antibodies are transient, lasting only a few months. Thus a positive antibody test indicates a cat has been infected with heartworm recently (it does not tell us if the cat has adult worms in its system or not) and a negative test doesn’t really indicate much at all. Running both the antibody and antigen tests in cats is the best way to detect heartworm infection, but even the combination of tests may miss infection in some cats.
Hookworms get their name from their hook-like teeth. Hookworms are one of the most dangerous intestinal parasites of dogs and cats because they feed on blood. These parasites use their sharp teeth to attach to the interior lining of the host’s intestine where they can consume copious amounts of blood. A heavy infestation of hookworms in a puppy or kitten can cause severe blood-loss anemia, leading to death.
These worms may move from one site to another in the intestine, leaving bleeding ulcers at each previous bite wound.
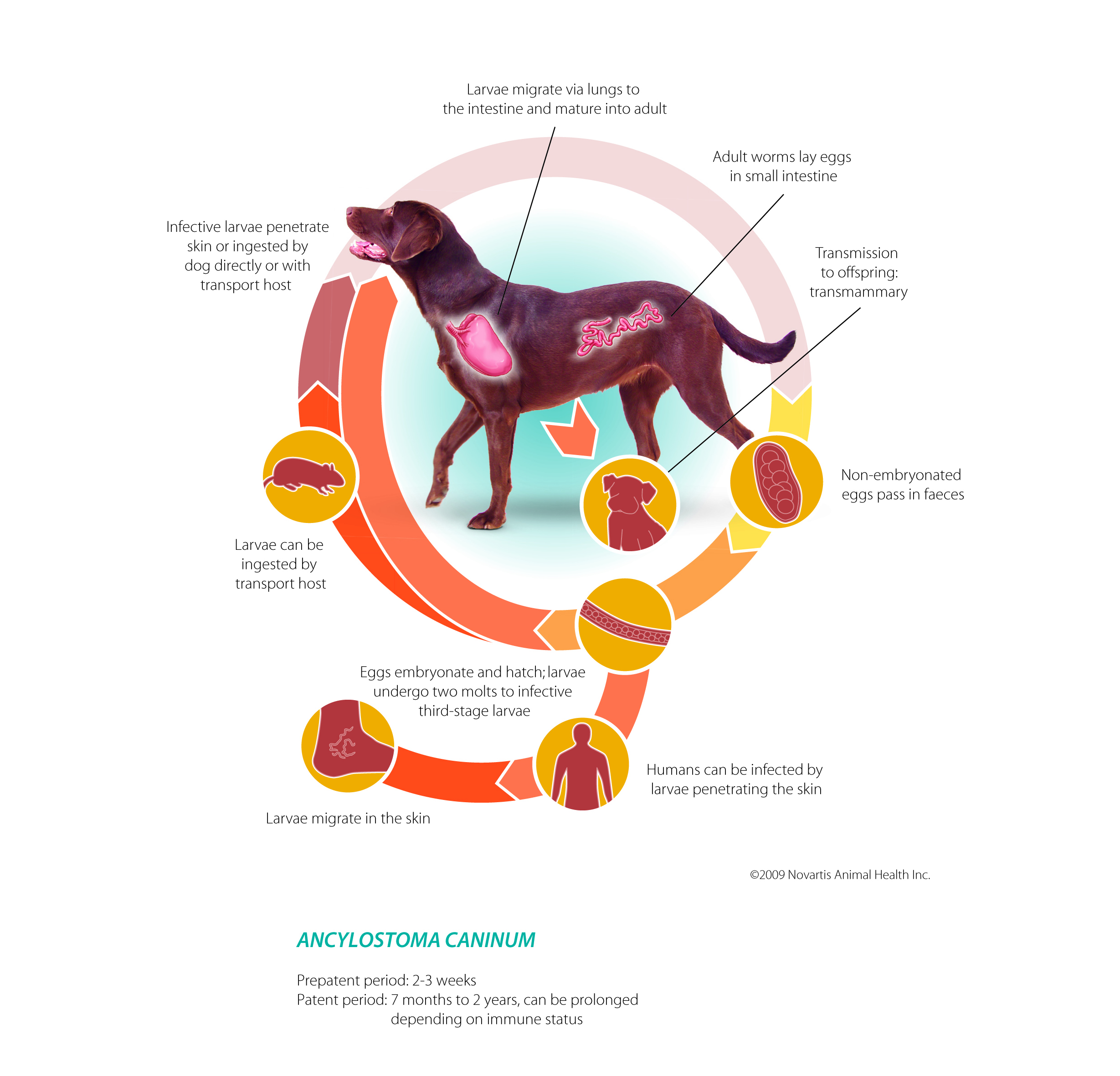
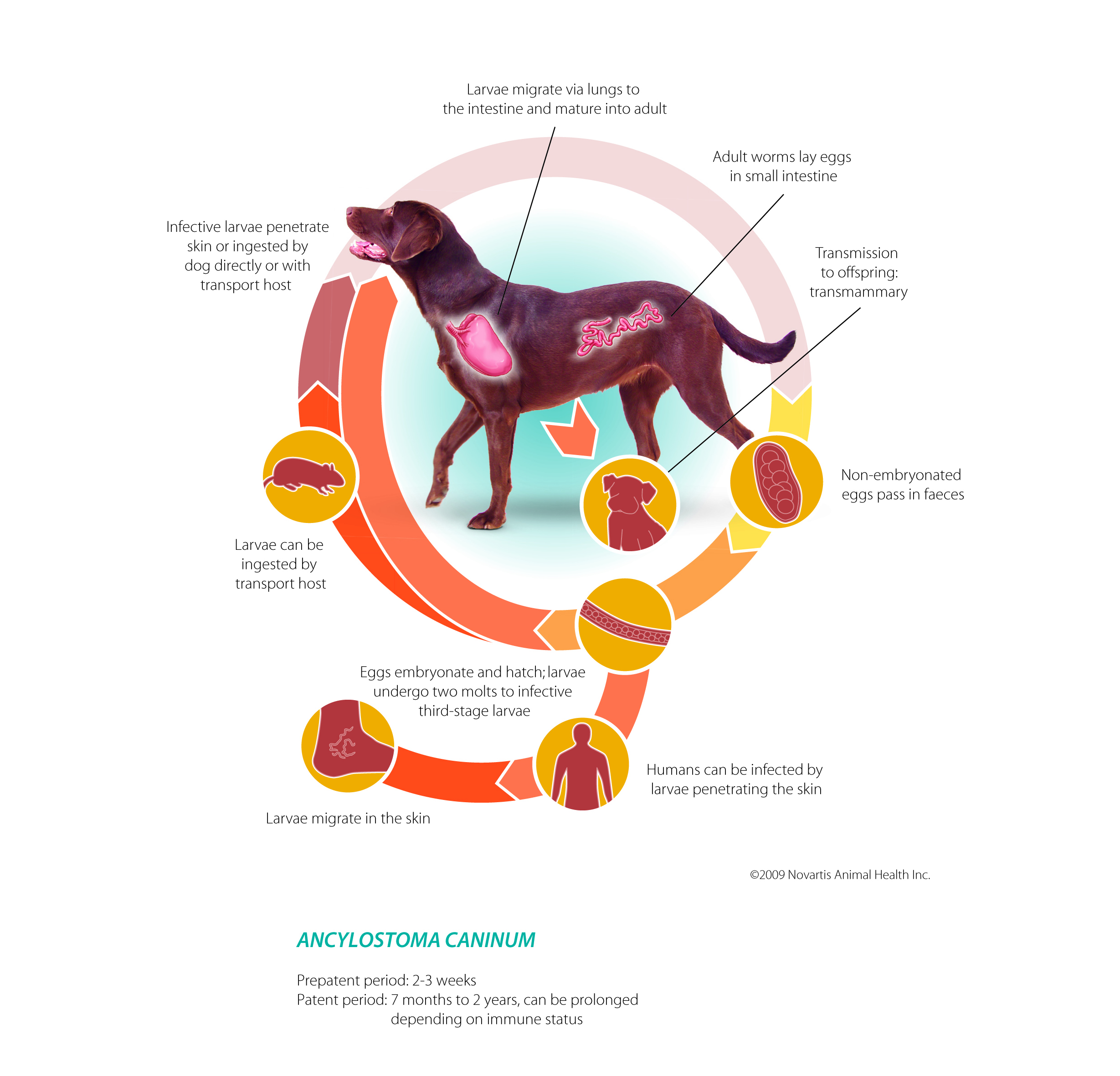
Hookworms are very common in dogs and cats. One subspecies of hookworms, Ancylostoma caninum, crosses the mammary tissue of the dam and infects puppies as soon as they nurse. Kittens are usually infected through the environment. Because they are so common, all puppies and kittens should be routinely dewormed early in life. Hookworms are very small and are very difficult to see with the naked eye. It is rare that a pet owner identifies these worms in the animal’s stool. They are more easily identified through laboratory testing.
There are several ways an animal can be infected with hookworms. Puppies are most often infected while nursing. The larval worm from the dam passes through the mammary gland and into the milk and is ingested by the baby. Puppies and kittens as well as adult animals can also be infected by ingesting the larva of the hookworm. Eggs are passed in the stool of infected animals, which then develop into infective larva in the environment. These larva may be ingested, but they also have the ability to invade the skin of pets (and humans) who come in contact with contaminated soil. The larva then migrate to the intestine where they complete their life cycle. Finally, dogs and cats can become infected if they eat another infected animal. Even 100% indoor pets are at risk, as some insects pests (e.g. cockroaches) can carry infective larva and may be eaten by the pet inside the home.
Hookworms are a zoonotic disease, meaning people can also be infected.
Hookworms are a zoonotic disease, meaning people can also be infected. Infection most often occurs when the larva of the worm comes in contact with exposed skin when the person digs or walks barefoot through contaminated soil. Humans are not the normal host for these worms, but they can cause a severe skin irritation when the larva migrate through the skin. Thankfully, the hookworm cannot complete its life cycle in a person, and the larva will die within the skin after several weeks. Treatment by a physician can shorten the course of disease. In people, the disease is called Cutaneous Larva Migrans. Thorough hand-washing after outdoor activities and wearing shoes anywhere infected animals may have been will help prevent transmission.
The life cycle of a hookworm takes approximately three-four weeks to complete.
A diagnosis of hookworm infection is made by fecal floatation. Treatment is usually effective and straightforward. Treatment generally consists of a general dewormer and environmental cleaning. Indoors, the floor should be vacuumed and cleaned with an all-purpose cleaner. Litter boxes and bedding should be scrubbed and laundered. All animals in the house should be dewormed together to ensure all infected animals are treated. All stool should be removed from outdoor areas, and care should be taken to avoid visiting areas where large numbers of animals visit, as soil in these environments may harbor parasite eggs for many years.
Thankfully, prevention is easy. Most monthly heartworm preventions for dogs and cats also protect against hookworm infection. These products work by eliminating any parasites the animal has contracted within the last 30 days, so it is important to use them regularly year-round for full protection. Animals who have not been on routine heartworm prevention can be dewormed with a general dewormer. Annual or bi-annual fecal floatation testing should also be performed to ensure no failure of preventative medications.
For more information on hookworms, visit the Companion Animal Parasite Council’s (CAPC) webpage on hookworms.
The disease is commonly referred to as “Lepto,” and can cause kidney and liver failure. Leptospirosis is a zoonotic disease, meaning it can be passed from animals to humans.
Symptoms
The ticks typically pick up the bacterial disease from wildlife, and then when they feed on your pet, they transfer the disease. In order for the disease to be transferred to your pet, the tick needs to be attached for at least 48 hours. However, the ticks that carry the disease are often very small and difficult to find, which makes it that much more important to have your pet on both a tick preventative and vaccinated.
Unlike with humans, dogs do not typically develop the “bulls-eye” rash. The lack of a physical indicator of being bit by a tick, coupled with the fact that many dogs do not show symptoms of Lyme disease right away (or at all). However, this do not mean that the disease does not exist.
If a pet is positive for Lyme disease, antibiotics can be given to try to eliminate as much of the bacteria in the body. It is difficult to completely eliminate the bacteria in the body, so even with a course of antibiotics helping symptoms, a low-level infection may always be present.
Symptoms
- some dogs can show no symptoms at all (asymptomatic)
- pain
- limping
- lameness
- inappetence
- fever
- in severe cases, kidney and heart disease can develop
While Borelia Burgdorferi can infect multiple species of tick, only the black-legged tick (also known as the deer tick) and the Western black-legged tick have been shown to transmit the disease to other hosts. Transmission occurs 24-48 hours after a tick attaches to its host. Ticks find and bite a host and attach by embedding a feeding tube into the host’s skin. The tick then secretes a small amount of saliva through the feeding tube which anesthetizes the skin and prevents the host from detecting the tick. As the tick feeds, it continues to secrete saliva into the wound. 24-48 hours after feeding begins, the Lyme bacteria mobilizes and enters the host through this saliva secretion.
Most dogs who become infected with the Borelia Burgdorferi bacteria do not develop clinical signs of Lyme disease. Instead, they are infected subclinically, meaning they carry the bacteria but do not get sick from it. Dogs that do develop clinical signs of Lyme are likely to exhibit a combination of fever, lameness and general malaise. Less commonly, the Lyme bacteria can infect the kidneys, causing significant protein loss through the kidneys which eventually leads to kidney failure. In very rare cases, Lyme disease can cause heart or brain disease.
Lyme disease is treated with antibiotics and supportive care. Although antibiotic treatment is often successful in resolving clinical signs of disease, low-levels of bacteria generally remain in the body and infected patients may continue to test positive for Lyme infection long-term. Persistently infected dogs may have a recurrence of clinical signs during times of stress or immunosuppression (for example, during cancer treatment or treatment of autoimmune disease).
The best way to protect your pet is to prevent Lyme disease transmission in the first place. Tick control is the first line of prevention. Keep your pet on a high-quality tick preventative year-round to limit his exposure. Secondly, a Lyme vaccine is available to help your dog fight of the Lyme bacteria if he is bitten by a tick. This vaccine is given annually after the initial two-booster series. Finally, your veterinarian may recommend antibiotic treatment after a recent tick bite to try and kill any transmitted bacteria before they can establish an infection in your pet.
Caring Hands Animal Hospital recommends annual testing of dogs for Lyme disease using our in-house Heartworm/Lyme/Ehrlichia/Anaplasmosis test. This test is the most accurate way to screen for Lyme infection. If the dog tests positive, your veterinarian may recommend additional testing and/or a course of antibiotics. Dogs who have tested positive in the past should be tested using a send-off test called the Lyme C6. This test measures the amount of Lyme antibody in the dog’s body and is an accurate way to measure the number of Borelia Burgdorferi bacteria present. If this number is rising, re-treatment with an antibiotic may be needed.
Lyme disease affects people as well as animals. Although the disease is not transmitted directly from animals to people, people can be infected by the bite of an infected tick. At the current time, there is not an effective Lyme vaccine available for people. Thus, tick prevention is the best method of preventing Lyme disease in people.
For more information on Lyme, see the links below:
The disease is transmitted through the saliva of an infected animal, usually through a bite.
Vaccination is required by Virginia state law for all dogs and cats.
Symptoms
The Library of Terms
Easily transmitted through direct contact or the air; vaccination is recommended for all dogs that interact with other dogs in their neighborhood, boarding and daycare facilities, dog parks, and groomers.
Unvaccinated puppies or young dogs, and dogs that have a compromised immune system may experience severe symptoms.
Symptoms
- a dry, hacking cough
- “honking” cough
- nasal discharge
- decrease in appetite
- lethargy
- fever
A vaccine was developed to help protect dogs and is available if needed. It was found to not be contagious to humans.
Symptoms
The Influenza vaccine is given as a series of two, and then annually to adult and senior dogs.
The disease is spread through both direct and indirect contact.
Symptoms
For dogs, the vaccine offers protection from intestinal viruses including Distemper, Hepatitis, Parainfluenza, and Parvovirus.
For cats, the vaccine offers protection from upper respiratory viruses including Rhinotrachitis, Calicivirus, and Panleukopenia.
These vaccines are often abbreviated to DHPP and FVRCP.
Distemper vaccines are given as a series to puppies and kittens, annually to young adult pets, and every 3 years in older adults and seniors.
Nursing kittens, feral or outdoor cats, and cats living in multi-cat households are at risk of infection. There is currently no known cure for Feline Leukemia.
A blood work screen can be completed in hospital to determine if a patient is infected with Feline Leukemia.
Symptoms
There are many different types of flea and/or tick preventatives on the market today. We understand that it can be difficult to keep up with all of the brands, application methods, and pros/cons of them all. Here is a guide on the different types of preventives available with information about how they are applied, pros and cons for each one, and some things to think about when deciding if it is the right option for you and your pet.
When choosing a flea/tick preventative it is important to consider you and your pet’s lifestyle. There are many factors that could contribute to the decision of which option is best for you. Age, species, breed, health status, and any current medications should all be considered. All of the flea/tick preventatives are medications and any new products should not be started without first talking with your veterinarian.
The most popular form of flea/tick preventative is a topical medication, often referred to as “spot on” products. These are usually applied at the base of the neck or between the shoulder blades. They contain ingredients that kill fleas and ticks. Some products also contain a repellant quality that adds an additional layer of protection of keeping the pests off your pet in the first place. Topical preventatives spread over the pet’s body either through sweat glands or using a bioadhesive. It is generally convenient to use, and once dried, the pet is able to go swimming or be bathed. It is important to note that the product should be allowed to dry, and that it is important to keep kids and other pets away until fully dried. Also, be sure to bathe your pet with gentle shampoos that do not strip the skin. This could cause the medication to be removed as well. Possible side effects include itching/scratching, redness or swelling of the skin, or hair loss.
Oral medications are becoming more popular, as it takes away the worry of getting the topical medication on and letting it dry. None of the oral medications available have the ability to repel fleas or ticks, requiring the parasites to bite/attach before they will be killed. As with any oral medication, there is a risk of upsetting the stomach or the pet not taking the medication (either refuses to eat it outright or takes it and spits it out later… behind a couch). Possible side effects include vomiting and diarrhea, as well as some skin reactions like redness, itching, and/or hives. Depression and a decreased appetite have also been reported.
In addition to everything listed above, some topical and oral products can also prevent heartworm disease in dogs and cats. It is important to evaluate what each product covers to determine if you are getting the appropriate protection for your pet and their lifestyle
Collars are also popular since they can just be put on the pet and the owner doesn’t have to worry about a liquid product drying or giving the pet an oral medication. Collars contain a concentrated chemical that can kill and repel fleas and ticks. These are relatively inexpensive, but some of them can smell quite strong and can be irritating to the pet. There is also risk in humans touching the collars, especially children.
Sprays are also available, but can be difficult to apply for complete coverage. The pet has to stay dry for these to work also, which makes it difficult for baths, swimming, or even walking in the rain. It is important to remember when applying these to avoid the pet’s eyes and mouth.
Powders are dusted over the body and rubbed into the fur. Again, it can be difficult to get complete coverage and it is important to avoid the pet’s eyes and mouth. Side effects can include vomiting, diarrhea, drooling, depression, and decreased appetite.
Shampoos are available to help wash away adult fleas and their eggs. This is a very short-term solution and will not be a preventative measure. The pet can still get fleas later on. When using, you should allow it to sit on the skin and coat for at least 15 minutes before rinsing well. Be sure to avoid getting the shampoo in the pet’s eyes and mouth.
Dips are similar to shampoos, whereas they are not a preventative, but a short term solution. They are usually a very concentrated liquid that is diluted with water and applied to the pet. They do not get rinsed and need to be air dried. Dips cannot be used on very young pets or on pets if they are nursing or pregnant. It is usually advised to have a dip done by a professional, as they are very concentrated and should be used with extreme caution. If you are administering a dip, it is important to protect your skin and eyes while applying to the pet. You should also avoid the pet’s eyes and mouth.
Some important questions for you, as the pet owner to consider:
Tips for using a flea/tick preventative:
Heartworms are carried by several species of mosquitos and are transmitted when the mosquito feeds. When a bite occurs, the larval heartworms migrate through the soft tissue to the blood vessels and then they travel to the heart and lungs. Once there, they mature into adult worms, sometimes reaching several inches in length. The adult worms then reproduce, sending offspring into the bloodstream. The next mosquito that bites ingests the larva, becoming infected and carrying the parasite to its next host.
The classic form of heartworm disease occurs in dogs and is easily diagnosed with a blood test. Dogs with the disease often have large numbers of adult worms living in the blood vessels of the lungs and in the heart. These worms partially block the flow of blood, acting like a dam in the vessels. When the dog is active, it may have trouble moving enough blood to bring oxygen to the tissues. The heart must work much harder than normal to move the same amount of blood, and over time this leads to heart disease. Additionally, when adult heartworms are a few years old, they die of old age. Dead worms cause significant inflammation in the surrounding lung tissue, leading to coughing and shortness of breath. As the disease progresses, poor oxygenation and advancing heart failure can lead to the death of the dog.
Cats are not the normal host for heartworms, but recent studies show that they are infected at nearly the same rate as dogs. Cats also contract the disease through the bite of an infected mosquito. The heartworms start their migration through the tissue and blood vessels to the lungs, but often die in the lungs before reaching full maturity. If adult heartworms develop in a cat, it is usually in low numbers. Despite this fact, the migration of larval worms through the lungs can cause severe and permanent damage. Studies have shown that infected cats, even those in which the worms die before reaching maturity, develop long-term inflammation and narrowing of the airways. These cats may cough, show shortness of breath, or die suddenly due to their disease. Feline heartworm disease mimics, and is often misdiagnosed, as asthma. This is because the clinical signs and radiographic findings are identical, and heartworm tests do not consistently identify infected cats.
Dogs who contract heartworm disease can be treated with injectable medications. The treatment is expensive and painful, and even when the worms are gone, the lungs may be permanently scarred. To date, a safe treatment has not been developed for cats. The best “treatment” for both dogs and cats is to prevent the disease all together. Monthly heartworm prevention medications are available for both dogs and cats through your veterinarian. These preventatives are inexpensive, effective, and safe. All dogs and cats should receive monthly preventatives, even those who never go outside. This is because mosquitos commonly invade houses. Studies have shown that all indoor cats are at nearly equal risk for heartworm infection as cats that spend time outdoors. Additionally, monthly preventatives should be continued year-round because some species of mosquitos that transmit heartworm disease are hardy even in the middle of winter when there are sub-freezing temperatures.
In the Northern Virginia area, heartworm infection rates (as measured in dogs, where the test can accurately detect infection) are higher than they have been in the last 10 years. Your pet doesn’t have to be one of those infected. Protect your pet year-round with a heartworm preventative every 30 days. For more information on heartworm disease, visit The American Heartworm Society.
In dogs, heartworm tests work by detecting antigens of the heartworm in the dog’s blood. A few drops of blood are mixed with the test solution, and then poured into the tester. The tester contains antibodies that bind to heartworm antigens (a protein produced in the female worm’s uterus). When this binding occurs, a colored dot develops indicating the animal is infected with heartworms. Because infected dogs have a large number of heartworms in their system, these tests are very accurate. However, in order for a dog to test positive on the test, it must have mature female worms in its system. Heartworms take heartworm-interpreting-results courtesy of Idexxapproximately 6 months to reach maturity after infection, so dogs with very early infections may still test negative on the test.
There are two types of tests available for cats. One is an antigen test similar to the one used in dogs. This test will turn positive if it detects antibodies of three or more adult female worms. However, most infected cats only have a few adult worms in their system (1-7 worms), and chances are high that all or most may be male. If this is the case, the test will be negative. Thus, a positive antigen test in a cat indicates it is truly infected with heartworms, but a negative test does not rule out the possibility of infection.
The second type of test available for cats is an antibody test. This test detects heartworm-specific antibodies circulating in the cat’s blood stream. Antibodies are produced by the cat’s body when heartworm larvae reach the L4 stage. However, these antibodies are transient, lasting only a few months. Thus a positive antibody test indicates a cat has been infected with heartworm recently (it does not tell us if the cat has adult worms in its system or not) and a negative test doesn’t really indicate much at all. Running both the antibody and antigen tests in cats is the best way to detect heartworm infection, but even the combination of tests may miss infection in some cats.
Hookworms get their name from their hook-like teeth. Hookworms are one of the most dangerous intestinal parasites of dogs and cats because they feed on blood. These parasites use their sharp teeth to attach to the interior lining of the host’s intestine where they can consume copious amounts of blood. A heavy infestation of hookworms in a puppy or kitten can cause severe blood-loss anemia, leading to death.
These worms may move from one site to another in the intestine, leaving bleeding ulcers at each previous bite wound.
Hookworms are very common in dogs and cats. One subspecies of hookworms, Ancylostoma caninum, crosses the mammary tissue of the dam and infects puppies as soon as they nurse. Kittens are usually infected through the environment. Because they are so common, all puppies and kittens should be routinely dewormed early in life. Hookworms are very small and are very difficult to see with the naked eye. It is rare that a pet owner identifies these worms in the animal’s stool. They are more easily identified through laboratory testing.
There are several ways an animal can be infected with hookworms. Puppies are most often infected while nursing. The larval worm from the dam passes through the mammary gland and into the milk and is ingested by the baby. Puppies and kittens as well as adult animals can also be infected by ingesting the larva of the hookworm. Eggs are passed in the stool of infected animals, which then develop into infective larva in the environment. These larva may be ingested, but they also have the ability to invade the skin of pets (and humans) who come in contact with contaminated soil. The larva then migrate to the intestine where they complete their life cycle. Finally, dogs and cats can become infected if they eat another infected animal. Even 100% indoor pets are at risk, as some insects pests (e.g. cockroaches) can carry infective larva and may be eaten by the pet inside the home.
Hookworms are a zoonotic disease, meaning people can also be infected.
Hookworms are a zoonotic disease, meaning people can also be infected. Infection most often occurs when the larva of the worm comes in contact with exposed skin when the person digs or walks barefoot through contaminated soil. Humans are not the normal host for these worms, but they can cause a severe skin irritation when the larva migrate through the skin. Thankfully, the hookworm cannot complete its life cycle in a person, and the larva will die within the skin after several weeks. Treatment by a physician can shorten the course of disease. In people, the disease is called Cutaneous Larva Migrans. Thorough hand-washing after outdoor activities and wearing shoes anywhere infected animals may have been will help prevent transmission.
The life cycle of a hookworm takes approximately three-four weeks to complete.
A diagnosis of hookworm infection is made by fecal floatation. Treatment is usually effective and straightforward. Treatment generally consists of a general dewormer and environmental cleaning. Indoors, the floor should be vacuumed and cleaned with an all-purpose cleaner. Litter boxes and bedding should be scrubbed and laundered. All animals in the house should be dewormed together to ensure all infected animals are treated. All stool should be removed from outdoor areas, and care should be taken to avoid visiting areas where large numbers of animals visit, as soil in these environments may harbor parasite eggs for many years.
Thankfully, prevention is easy. Most monthly heartworm preventions for dogs and cats also protect against hookworm infection. These products work by eliminating any parasites the animal has contracted within the last 30 days, so it is important to use them regularly year-round for full protection. Animals who have not been on routine heartworm prevention can be dewormed with a general dewormer. Annual or bi-annual fecal floatation testing should also be performed to ensure no failure of preventative medications.
For more information on hookworms, visit the Companion Animal Parasite Council’s (CAPC) webpage on hookworms.
The disease is commonly referred to as “Lepto,” and can cause kidney and liver failure. Leptospirosis is a zoonotic disease, meaning it can be passed from animals to humans.
Symptoms
The ticks typically pick up the bacterial disease from wildlife, and then when they feed on your pet, they transfer the disease. In order for the disease to be transferred to your pet, the tick needs to be attached for at least 48 hours. However, the ticks that carry the disease are often very small and difficult to find, which makes it that much more important to have your pet on both a tick preventative and vaccinated.
Unlike with humans, dogs do not typically develop the “bulls-eye” rash. The lack of a physical indicator of being bit by a tick, coupled with the fact that many dogs do not show symptoms of Lyme disease right away (or at all). However, this do not mean that the disease does not exist.
If a pet is positive for Lyme disease, antibiotics can be given to try to eliminate as much of the bacteria in the body. It is difficult to completely eliminate the bacteria in the body, so even with a course of antibiotics helping symptoms, a low-level infection may always be present.
Symptoms
- some dogs can show no symptoms at all (asymptomatic)
- pain
- limping
- lameness
- inappetence
- fever
- in severe cases, kidney and heart disease can develop
Lyme disease is the most common tick-borne disease in dogs and people in the United States. It is caused by a bacteria called Borelia Burgdorferi and is transmitted through the bite of an infected tick. Many species of mammals are susceptible to infection. In companion animals, dogs and horses seem to be the most likely to develop clinical signs from Lyme disease, while cats seem to be naturally resistant to infection. Lyme is most prevalent along the east coast and Great Lakes regions of the United States, but is found in many other areas of the country as well.
While Borelia Burgdorferi can infect multiple species of tick, only the black-legged tick (also known as the deer tick) and the Western black-legged tick have been shown to transmit the disease to other hosts. Transmission occurs 24-48 hours after a tick attaches to its host. Ticks find and bite a host and attach by embedding a feeding tube into the host’s skin. The tick then secretes a small amount of saliva through the feeding tube which anesthetizes the skin and prevents the host from detecting the tick. As the tick feeds, it continues to secrete saliva into the wound. 24-48 hours after feeding begins, the Lyme bacteria mobilizes and enters the host through this saliva secretion.
Most dogs who become infected with the Borelia Burgdorferi bacteria do not develop clinical signs of Lyme disease. Instead, they are infected subclinically, meaning they carry the bacteria but do not get sick from it. Dogs that do develop clinical signs of Lyme are likely to exhibit a combination of fever, lameness and general malaise. Less commonly, the Lyme bacteria can infect the kidneys, causing significant protein loss through the kidneys which eventually leads to kidney failure. In very rare cases, Lyme disease can cause heart or brain disease.
Lyme disease is treated with antibiotics and supportive care. Although antibiotic treatment is often successful in resolving clinical signs of disease, low-levels of bacteria generally remain in the body and infected patients may continue to test positive for Lyme infection long-term. Persistently infected dogs may have a recurrence of clinical signs during times of stress or immunosuppression (for example, during cancer treatment or treatment of autoimmune disease).
The best way to protect your pet is to prevent Lyme disease transmission in the first place. Tick control is the first line of prevention. Keep your pet on a high-quality tick preventative year-round to limit his exposure. Secondly, a Lyme vaccine is available to help your dog fight of the Lyme bacteria if he is bitten by a tick. This vaccine is given annually after the initial two-booster series. Finally, your veterinarian may recommend antibiotic treatment after a recent tick bite to try and kill any transmitted bacteria before they can establish an infection in your pet.
Caring Hands Animal Hospital recommends annual testing of dogs for Lyme disease using our in-house Heartworm/Lyme/Ehrlichia/Anaplasmosis test. This test is the most accurate way to screen for Lyme infection. If the dog tests positive, your veterinarian may recommend additional testing and/or a course of antibiotics. Dogs who have tested positive in the past should be tested using a send-off test called the Lyme C6. This test measures the amount of Lyme antibody in the dog’s body and is an accurate way to measure the number of Borelia Burgdorferi bacteria present. If this number is rising, re-treatment with an antibiotic may be needed.
Lyme disease affects people as well as animals. Although the disease is not transmitted directly from animals to people, people can be infected by the bite of an infected tick. At the current time, there is not an effective Lyme vaccine available for people. Thus, tick prevention is the best method of preventing Lyme disease in people.
For more information on Lyme, see the links below:
The disease is transmitted through the saliva of an infected animal, usually through a bite.
Vaccination is required by Virginia state law for all dogs and cats.
Symptoms

